
Electronic prior authorization (ePA)is gaining traction and attention after a lull in progress and focus.The need for ePA is easy to understand.ePA is essential in reducing timetotherapy, friction and costs by aligning payer and provider goals. The “how” is catching up in a big way. Now new technologies, evolving standards, government regulations andePA’srole as a critical tool for value-based care have created a perfect storm. The industry has brought ePA to an inflection point, and several leading payers, providers, vendors and standards groups are driving to advance ePA bymaking automated prior authorization (PA) the norm rather than the exception.
A way to conceptualize this progress is shown in the figure below. There are three phases in the evolution of ePA. The industry is rapidly transitioning from phase 1.0 and heading to phase 2.0.
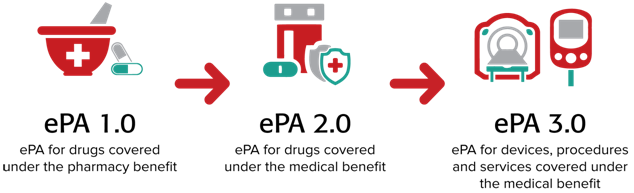
ePA 1.0. This first phase is focused on ePA for medications covered under a patient’s pharmacy benefit. Substantial progress has been made and is ongoing. Take, for example, the latest version of the SCRIPT standard by the National Council for Prescription Drug Programs (NCPDP). NCPDP SCRIPT version 20170701 contains ePA transactions that are more robust than those contained in the current ePA standard (ASC X12 278) and offer the ability for performing ePAs in real time.
Adoption of the NDPDP standard will be reinforced with the newly proposed rule from the Centers for Medicare and Medicaid Services (CMS), which would require use of ePA transactions contained in NCPDP SCRIPT 20170701 for drugs prescribed under Medicare Part D instead of the ASC X12 278. The proposed implementation date is January 1, 2021.
Another CMS rulewillsupport andaccelerateuse of the real-time pharmacy benefit check (RTPBC). The rule requiresadoption of a “Real-Time Benefit Tool” by Medicare Part Dplans beginning January 1, 2021. NCPDP has developed a draft standard for this transaction, whichwas approved to move forward at the August 2019 workgroup meeting.
With the RTPBC, bothprescriber and patient can have up-to-date information on the out-of-pocket costs of a drug that is being prescribed as part of the electronic prescribing (ePrescribing) process at the point of care through the electronic health record (EHR). When used with ePA, the two transactions deliver more accurate information about coverage and costs of drugs at the point of prescribing and allow physicians to help their patients begin therapy faster. The newly proposed ePAtransactions would enable the prescriber to submit the required information in real time and indicate in the RTPBC whether PA is needed. This will help the physician obtain faster approval and improve speed to therapy.
Improving the quality of the signal for PA through RTPBC will bolster the accuracy and utility of ePAas part of the prescribing process, such as support from industry groups such as the American Medical Association,which continues to support adoption of ePAas a way to reduce physician burden.
Taking ePA to Level 2.0.ePA 2.0 involves automating PAs for drugs covered under apatient’s medical benefit (mPA), such as drugs covered under Medicare Part B. Reducing provider burden isan increasing focus from the Department of Health and Human Services, including notices of proposed rulemakingthat would increase the ability for payers to share coverage decisions as members change plans and make continued investments in emerging technologies that can expose coverage rules to providers in their workflow.
Currently, most PAs for those medications are processed manually through antiquated phone, fax and paper processes. There are several drivers propelling ePA to the next level. These are being addressed by various stakeholder initiatives. For example:
- Specialty pharmacy. A large driver for mPA is the rapid growth of expensive specialty medications.Specialty medications are the fastest growing segment of the nation’s drug spend, primarily due to their high costs and use in addressing the large and expanding patient populations with chronic diseases.The government estimates that 60% of Americans have a chronic disease and 40% have two or more chronic conditions.
At the same time, prescribing specialty medications generally is a manual process, leading to provider frustration and reduced speed to therapy. Automating and standardizing specialty pharmacy transactions will be the focus of a new workgroup that has been formed by NCPDP. The goal is to bring greater focus and coordination in how NCPDP standards are used for the electronic exchange of data in specialty pharmacy, including addressing gaps that exist in ePrescribing for specialty medications. This will complement and support ongoing NCPDP efforts to automate various aspects of specialty pharmacy, including the patient enrollment process. In addition, NCPDP and HL7 are working together to use Fast Health Interoperability Resources (FHIR) to extract the necessary clinical data required for enrollment from the native EHR.
- Administrative burdens. Three-quarters of physicians (specialists and primary care) report the burden of PA is high. According to the American Medical Association, doctors and their staff spend the equivalent of nearly two business days navigating PA. Because this administrative burden is so great, about a third of physicians maintain staff members who exclusively deal with PAs. It usually takes days —even weeks — for an insurance company to decide whether it will approve a PA request. Needless to say, this leads to delays in therapy and frustration for both patients and providers. These factors are increasing the demand by provider associations for an mPA solution
- Costs.Significant administrative costs are associated with PA. Research by the Council for Affordable Quality Healthcare reveals that each manual prior authorization for medical care costs $3.50 for plans and $6.61 for providers. Going electronic brings that down to $2.80 per transaction for payers and $0.03 for providers. All in all, the study found that transitioning to electronic medical prior authorization could create $278 million in annual savings for providers and $139 million for health plans.
- Da Vinci. Significant investment from CMS, payers, providers and vendors is underway to accelerate adoption of ePA leveragingapplication program interface (API)-based standards. HL7’s FHIRis the basic building block for the HL7 Da Vinci Project—a private, multistakeholder initiative — with a number of use cases including PA. Da Vinci’s open business model process enables payers, health systems and other industry participants to identify and enumerate use cases that involve managing and sharing clinical and administrative data among industry partners. Coverage Requirements Discovery, an early use case, leverages a FHIR-based API that enables care delivery organizations and providers to query payers in realtime to find relevant guidance prior to care delivery to increase efficient delivery of care and corresponding payment. Building further, Documentation Templates & Rules enables providers to understand coverage requirements for a particular patient at the plan level, and work is underway to map the necessary clinical data required to automate the PA request itself with Prior Authorization Support. These use cases were tested at HL7’s September Connectathon in Atlanta.
To be sure, this new tranche of work is early, but stakeholders are ramping up to enable their platforms for API access so ePA can move to the next level.
Moving to ePA3.0.ePA 3.0 will automate PA fordevices, procedures and services covered under the medical benefit. Electronic medical prior authorization is in its early phases, but real work is underway with significant interest and attendance at Da Vinci working sessions and Connectathon activities.Many challenges must be addressed to bring ePA to version3.0. For example:
- The quality of provider data varies by vendor and payer capabilities. Payers will need to streamline and combine how pharmacy and medical claims are processed, as well as increase the accuracyand availability of PA requirements and benefit detail in workflow in real time.
- The increasing complexity of plan design, high-deductible plans, and members in at-risk contracts is increasing pressure on plans to improve available provider tools. Consensus will be needed on what those tools should be, the standards to support the underlying business design and how they will be handled in workflows.
- Refinements are needed in EHRs to support mPA. The ability to seamlessly share or identify in real time existing data locked into EHRswith APIs or data to createnecessary attachments must be addressed. EHRs still provide little or no support for PA, except for enabling attachmentsusing existing HIPAA-named standards. Creating a clear path for implementers from FHIR to other ePA standards is critical.
Edited by
Maurice Nagle